When my daughter Jessica was around 11 months old the rattle in her nose got worse and then turned to very bad congestion that wouldn’t go away. Then she got a strange rash on her back that continued to get bigger. At the same time she was getting low grade temperature’s up to 99.7.
I did a little research on vitamin C for kids from the book Superimmunity for Kids and found the following:
Dr. Leo Galland author of Superimmunity for Kids: What to Feed Your Children to keep them healthy now and prevent Disease in their future said about vitamin C, “Vitamin C in high doses is also an effective antihistamine. The doses that can produce this effect, 500 to 5000 mg. a day, are quite safe, even for toddlers, and vitamin C come in chewable tablets. The main side effect of an excess of either magnesium or vitamin C is diarrhea, which will stop when the dosage is reduced.” Pg. 132
Dr. Galland recommends about 500 mg. of vitamin C every three hours for a cold or viral infection. I never did give Jessica that much when she was under two years old. When she got a bad rash on that covered half of her back when she was being exposed to high levels of mold, I gave her 500 mg. 3x a day. I have increased that as she has gotten older and only when a cold lingers a long time. The most she has gotten is 2500 mg. of vitamin C in a day. Dr. Galland recommends that if you have recurrent or chronic respiratory infections that 500 mg. of vitamin C a day is good for a 1-3 year old. Jessica has other issues that deplete vitamin C including allergies and a genetic histamine issue.
Dr. Galland says, “In allergies, as in recurrent infections, deficiencies in certain nutrients contribute to a malfunction of the immune system.
Dr. Galland recommends a few things for colds and other viral infections but the vitamin C recommendations are, “give him vitamin C about 500 mg. every three hours. If his bowels become loose, stop giving it that day. the next day, give him 200 milligrams every three hours. If his bowels again become loose, stop vitamin C that day; the next day, give him 100 mg. every 4 hours. Then give him about 500 mg. a day until he’s recovered…although some claim that megadoses of vitamin C are not utilized by the body and are just excreted in the urine, vitamin C in doses of 1,000mg a day or more has been shown to enhance immune function in normal human volunteers.” Pg. 124
One concern about high doses of vitamin C could be oxalates or calcium oxalate stones or kidney stones. The following is a quote from a book entitled, Curing the Incurable; vitamin C, infectious diseases, and toxins by Thomas E. Levy, M.D. JD. “One of the primary reasons why the vitamin C/kidney stone connection continues to generate concern is because vitamin C does increase the urinary concentration of oxalate. Therefore, it just seems logical to assume that more and prolonged vitamin C administration will continue to increase this concentration until calcium oxalate stones begin to form…however, research proves that this is not the case, although vitamin C is one of many risk factors for increased oxalate formation and the subsequent formation of calcium oxalate stones. Schmidt et al. (1981) determined that there was actually a leveling off of oxalate production even though vitamin C dosing was continued. The researchers noted that a significant amount of the vitamin C does not even get metabolized to oxalate and is excreted unchanged in the urine…when very high doses of vitamin C are administered for any significant medical condition, the active, non-oxidized form of vitamin C is much more readily regenerated from the oxidized vitamin C than the metabolic breakdown products. This process further inhibits the irreversible metabolism of vitamin C to the oxalate end product. Takeouchi et al. (1966) noted that about 80% of vitamin C administered to human subjects was eliminated as dehydroascorbic acid, the oxidized form of vitamin C. They concluded that the metabolic breakdown of vitamin C in humans does not necessariliy have to follow the entire sequence down to oxalate. They also noted that as the vitamin C dose is increased, urinary excretion of diketogulonic acid increased. This is a clear indication that further oxidative breakdown of the diketogulonic acid to oxalate does not have to occur for a metabolic breakdown product of vitamin C to be excreted.”
He further states, “Logically, there have to be multiple other ways to metabolize and excrete vitamin C rather than by urinary oxalate. Casciari et al., (2001) showed that 50,000mg daily doses of intravenous vitamin C have already been given to cancer patients for eight-week periods without problem. If urinary oxalate was the only excreted metabolic product of vitamin C, such doses would cause such a supersaturation of oxalate in the urine that crystal deposition and eventual stone formation would have to occur. Yet, this does not occur.” Pg. 381-382
Since it is logical to think that this author is talking about adults and the above doses are extremely even for adults. I wanted to point out that Dr. Levy includes studies showing that vitamin C is even safe for premature infants saying, “In an article reviewing a large number of vitamin C studies, Hanck (1982) also confirmed the remarkable safety of long-term supplementation. Bass et al. (1988), in a double-blind study, found that vitamin C administration was very safe even for premature infants.” Pg. 374
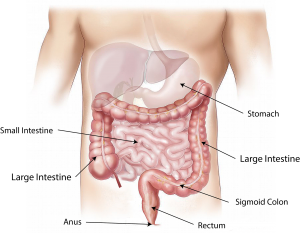
Dr. Levy includes a list of risk factors involved in precipitation of calcium oxalate out of the urine, leading to stone formation. He includes a few that stood out to me in thinking about our situation with my daughter, calcium ascorbate as the type of supplemental vitamin C, vitamin D supplementation, intake of oxalate stone generating or oxalate containing beverages (we drink fermented drinks like fermented coconut water and kombucha, intake of oxalate stone-generating toxins (Jess was exposed to toxic mold, and Crohn’s disease itself (we don’t know what kind of IBD Jess may have.
I looked up the study that Levy quotes about renal stones and IBD and it says in part, “RESULTS: Renal calculi were found in two patients with CD and in none with UC. Hyperoxaluria was present in 36% of patients with CD but was absent in those with UC. Analysis of covariance showed an association between low urinary citrate/creatinine ratio and renal stones (P=0.02), and between a combined urinary citrate and magnesium deficit relative to calcium, as expressed in the CMC index (citratexmagnesium)/calcium), and renal stones (P=0.017). Changes in urinary calcium, oxalate, urate, magnesium or the calcium oxalate index were not associated with the presence of stones. There was no independent relationship between any clinical factor and the presence of stones. CONCLUSION: Lower urinary concentrations of magnesium and citrate (stone inhibitors), relative to calcium (stone promoter; the CMC index) may be more important in lithogenesis in inflammatory bowel disease than is hyperoxaluria. In patients with a functioning colon, a low CMC index may predict likely stone-formers; this requires a prospective evaluation. Avoiding low urinary levels of magnesium and citrate may aid in preventing and treating renal calculi.” https://www.ncbi.nlm.nih.gov/pubmed/12010224
In my research about IBD I have found more information about vitamin deficiencies and the need for supplementation than the other way around. See the following study about that, “A case of scurvy presenting in a patient with Crohn’s disease is reported. A normal response to replacement therapy is seen. Vitamin C (ascorbic acid) deficiency was found in 7 out of 10 patients with clinically quiescent Crohn’s disease, 4 of whom had an adequate oral intake of vitamin C. There was no significant difference in oral intake between patients with Crohn’s disease and matched controls but there was a significant difference (P less than 0.001) in leucocyte ascorbic acid levels. It is recommended that patients with Crohn’s disease be screened for vitamin C deficiency and receive prophylactic vitamin C supplements daily. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2425408/
It seems to me that Jessica should be more carefully monitored for her vitamin status and supplemented as necessary given her restricted diet. The OAT (Organic acid) test from 1 year ago did not show specifically a vitamin C deficiency but it did for multiple B-vitamins including B6, B12, and B1. That test from what I can tell did not look at magnesium which I think we should look at.
Have you had any side effects or experience with Vitamin C, please share, it could help someone else.